The Importance of Addressing Drug Resistant Bacteria
Drug resistant bacteria, also known as antimicrobial resistant (AMR) bacteria, are a pressing global health threat that affects millions of people each year. As bacteria evolve and develop resistance to commonly used antibiotics, the effectiveness of medical treatments diminishes, leading to longer hospital stays, higher medical costs, and increased mortality rates. The World Health Organization (WHO) has warned that without effective strategies to combat this issue, we may face a return to a time where routine surgeries and minor infections can once again become life-threatening.
The Current Landscape
According to the Centers for Disease Control and Prevention (CDC), at least 2.8 million infections in the United States each year are caused by resistant bacteria, and nearly 35,000 people die as a result. In Canada, a report from the Canadian Antimicrobial Resistance Surveillance System (CARSS) indicated about 14,000 healthcare-associated infections occur annually due to drug resistant pathogens. The recent COVID-19 pandemic has further exacerbated the situation, as the overuse of antibiotics during treatment of viral infections has contributed to increased resistance.
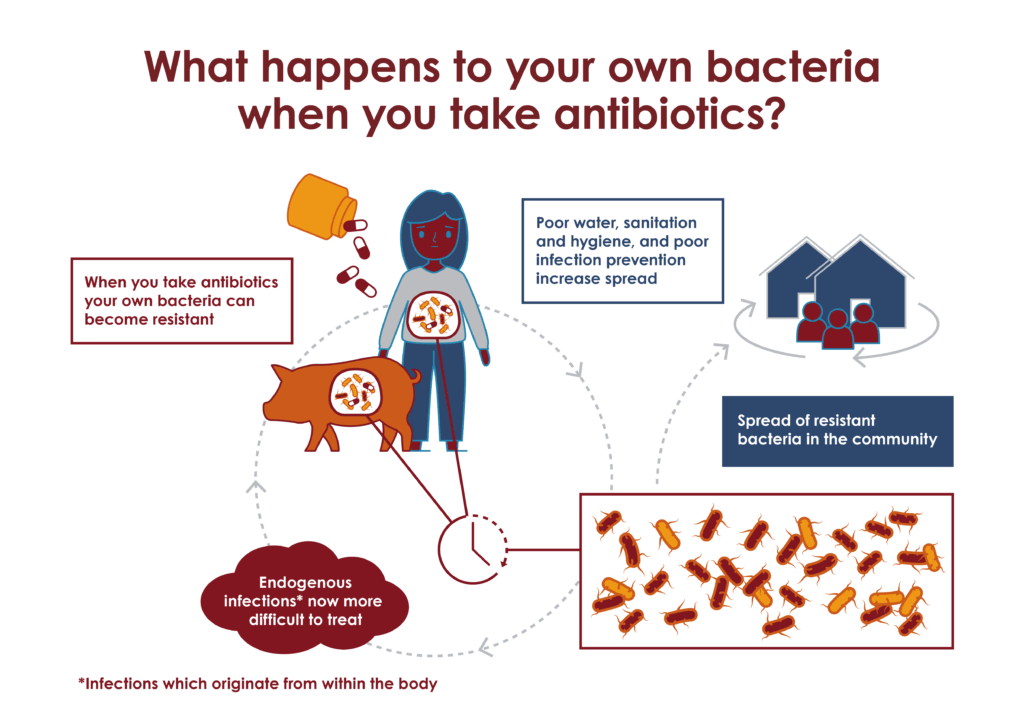
Key Factors Contributing to Resistance
Several factors contribute to the rise of drug resistant bacteria. Over-prescription and misuse of antibiotics, particularly in healthcare and agriculture, play a crucial role. Patients often demand antibiotics for viral infections, and healthcare providers may succumb to this pressure. Additionally, the routine use of antibiotics in livestock farming to promote growth has significant implications for the development of resistant strains. Public health experts emphasize the need for improved surveillance and stewardship programs to combat these practices.
Future Strategies and Solutions
Efforts to tackle the crisis of drug resistant bacteria must be multifaceted. Raising public awareness about the responsible use of antibiotics and fostering better communication between healthcare providers and patients is essential. Furthermore, funding for research into new antibiotic alternatives and innovations, such as bacteriophage therapy and vaccines, is critical. Collaborative efforts at the international level, like the Global Action Plan on Antimicrobial Resistance, aim to strengthen national responses to this mounting challenge.
Conclusion
Drug resistant bacteria represent one of the most significant challenges to public health in the 21st century. As bacteria continue to evolve, our strategies must also adapt. By prioritizing education, responsible antibiotic use, and research into new solutions, we can combat this pressing threat and protect the efficacy of the antibiotics we have today for future generations. The time to act is now.



